Companies are under more pressure to analyze food samples for pathogens, but not all of them have the expertise to handle the complexity involved in laboratory analysis. In addition, companies don’t want to risk contamination throughout their facility. As a result, many are outsourcing these services to contract labs.
Changing Landscape for Selecting a Food Safety Contract Laboratory
Strategic Consulting, Inc. recently conducted a study of food processors and the trends in outsourcing their laboratory testing work to food contract laboratories. The firm spoke with 100 food processors nationwide in 15 food processing categories, including protein, dairy, vegetables and packaged foods, inquiring about the types of samples they collect, how many are collected on a daily and monthly basis, their target analytes, and where they have the analysis performed (an in-plant lab, central company lab or an outsourced food contract laboratory); the firm also spoke with folks at leading food companies and a number of large food contract labs.
Bob Ferguson, managing director at Strategic Consulting, shared his insights with Food Safety Tech about the survey, the details of which will be presented at the Food Safety Consortium in December.
Food Safety Tech: What were some of the major findings?
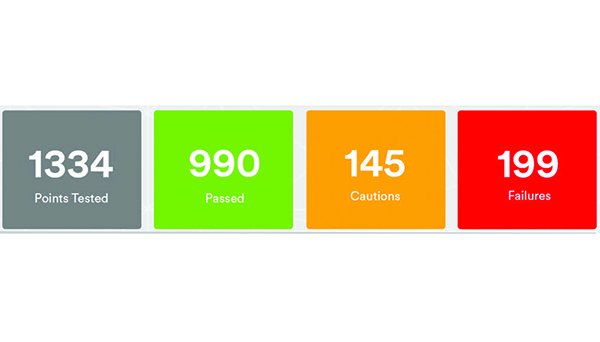
Bob Ferguson: Food processors continue to outsource more and more of their lab analysis. This is a trend that we outlined in our Food-8 market report in 2014, and it is clearly continuing and growing. The impact is particularly acute in microbiology testing, especially when analysis is for pathogens. Of the companies we surveyed, 87% did some amount of routine microbiology testing and 67% of those analyzed the samples at an in-house lab. But when asked about pathogens, 77% of the companies analyze samples for pathogens but only 34% analyze the samples at an in-house lab. Clearly there is a higher level of concern in handling pathogens at in-house labs.
Food Safety Tech: What are the processors’ concerns regarding pathogens?
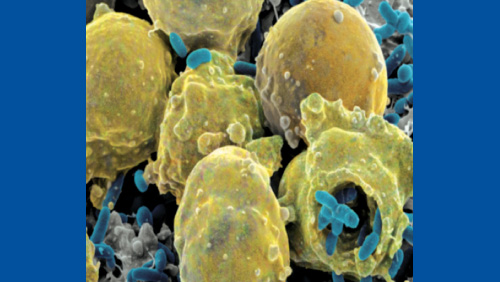
Ferguson: I would say that their concerns fall into two major categories: Technical and operational. From a technical perspective, there is always a risk when working with pathogens in a food processing facility. Microbiologists understand how easily bacteria can travel through a facility—being carried on employees, their clothing, or equipment, through air currents, or even through penetration connections such as drains. And most diagnostic tests not only require handling pathogen samples but also enriching the samples prior to analysis. The presence of food samples with high concentrations of pathogens can present a risk for the spread of contamination into production areas.
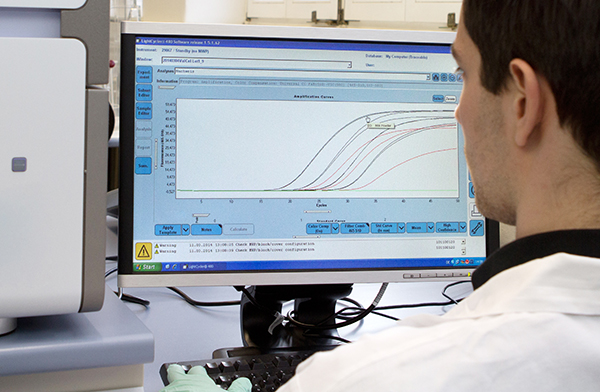
From an operational standpoint, running a food analysis lab is becoming increasingly more complex. Analytical methods continue to get more sensitive and sophisticated, and this requires more expertise and a greater focus on instrument service and calibrations. Requirements for accreditation of food testing laboratories are also raising the bar for in-plant labs. Finally, running a food lab requires recruiting and hiring skilled analysts. More food processors are coming to the conclusion that none of these functions are part of their core competencies and are electing to outsource that work to a contract lab.

Food Safety Tech: What does this mean for food contract labs?
Ferguson: This could become a significant business growth opportunity for food contract laboratories. As we indicated in our Food Contract Laboratory market report, microbiology is one of the largest business areas for most food contract laboratories, comprising, on average, approximately 52% of lab revenues and growing on average at 12% annually. The average lab also reports pathogen testing growth at more than 13%. This is remarkable in that the overall growth in sample volume is only growing 6%, so labs are clearly gaining a greater share of samples.
Food Safety Tech: Is this good news for the food contract laboratory companies?
Ferguson: Well, I would say that this will dramatically change the nature of competition and will be good news for some lab companies, namely those who can best adapt to the changing market conditions, but certainly not all. Our analysis shows, for example, that about 70% of pathogen samples outsourced are sent to a lab within 100 miles of the food processing facility. This bodes well for labs with a robust national network of locations. Single-location or limited-location labs may have trouble competing and will be acquired or otherwise may not survive. Also, as more samples get outsourced, the most efficient laboratories will have a competitive advantage. Our data also shows that outsourcing does not occur uniformly across all types and sizes of food processing companies, and laboratories may be at more or less risk depending on their customer mix or concentration in a particular food processing segment. Food contract laboratories that understand these factors will be in a better position to compete and thrive as the market changes.