The importance of food safety testing technologies continues to grow, as companies are increasingly testing their products for GMOs and pesticides, and pathogens and contamination. Last year the global food safety testing market had an estimated value of $12 billion, according to a recent report by Esticast Research & Consulting. Driven by pathogen testing technologies, the global food safety testing market is expected to experience a 7.4% CAGR from 2017–2024, hitting $21.4 billion in revenue in 2024, said Vishal Rawat, research analyst with Esticast.
With a CAGR of 9.3% from 2017–2024, rapid testing technologies are anticipated to lead the market. Testing methods responsible for this growth include immunoassays (ELISA), latex agglutination, impedance microbiology, immune-magnetic separation, and luminescence and gene probes linked to the polymerase chain reaction, said Rawat, who shared further insights about the firm’s market projections with Food Safety Tech.
Food Safety Tech: With the GMO food product testing market expected to experience the highest growth in the upcoming future, can you estimate the projected growth?
Vishal Rawat: The GMO food product testing market is estimated to generate a revenue of approximately $5.2 billion in 2016. The market segment is expected to witness a compound annual growth rate of 8.3% during the forecast period of 2017–2024. This is a global market estimation.
FST: What innovations are occurring in product testing?
Rawat: Nanomaterials and nanobased technologies are attracting interest for rapid pathogen testing. Sustainable technologies such as edible coatings or edible pathogen detection composition can attain a trend in the near future. Also, new rapid allergen testing kits are now emerging out as the latest food testing technology in the market, which are portable and easy to use.
FST: Which rapid pathogen detection testing technologies will experience the most growth from 2017–2024?
Rawat: New and emerging optical, nano-technological, spectroscopic and electrochemical technologies for pathogen detection, including label-free and high-throughput methods would experience the highest growth.
FST: What pathogen testing technologies are leading the way for meat and poultry in the United States?
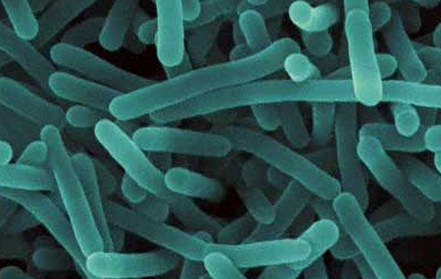
Rawat: The presence of a microbial hazard, such as pathogenic bacteria or a microbial toxin, in ready-to-eat (RTE) meat or poultry products is one basis on which these products may be found adulterated. The FSIS is especially concerned with the presence of Listeria monocytogenes, Salmonella, Escherichia coli O157: H7, and staphylococcal enterotoxins in RTE meat and poultry products. Rapid pathogen testing for E. coli O157:H7 and Salmonella, for ground beef, steak and pork sausages is going to lead the U.S. market.
An overview of the report, “Food Safety Testing Market By Contaminant Tested (Pathogens, GMOs, Pesticides, Toxins), By Technology (Conventional, Rapid), Industry Trends, Estimation & Forecast, 2015– 2024” is available on Esticast’s website.