As stated by CDC’s John Besser, Ph.D. last month at the Food Safety Consortium, “It’s been quite a year for outbreaks.” Here’s a not-so-fond look back at some of the noteworthy outbreaks and recalls of 2018.
Romaine Lettuce –E.coli O157:H7
2018 was not a good year for romaine lettuce. In the spring, a deadly multistate outbreak of E.coli O157:H7 was linked to romaine lettuce that came from the Yuma, Arizona growing region. “We knew right away that this was going to get bad and that it would get bad quickly,” said Matthew Wise, deputy branch chief for outbreak response at the Outbreak Response and Prevention Branch of the CDC at the 2018 Food Safety Consortium. Although the CDC declared the outbreak over at the end of June, the total number of illnesses had reached 210, with five deaths.
Then in November it was revealed that contaminated lettuce was coming from growing regions in northern and central California. According to the latest update from FDA, there have been 59 reported illnesses, with 23 hospitalizations, across 16 states. No deaths have been reported. Earlier this month Adam Bros Farming, Inc. recalled red leaf lettuce, green leaf lettuce and cauliflower, because it may have come into contact with water from the reservoir where the E. coli outbreak strain was found.
Raw Beef Products – Salmonella
At the beginning of the month, JBS Tolleson, Inc. expanded a recall of its non-intact raw beef products due to concerns of contamination with Salmonella Newport. More than 12 million pounds of product have been recalled. The latest CDC update put the reported case count at 333, with 91 hospitalizations across 28 states.
Shell Eggs – Salmonella
In April, Rose Acre Farms recalled more than 206 million eggs after FDA testing determined that eggs produced from the company’s farm were connected to 22 cases of Salmonella Braenderup infections. A total of 45 cases were reported across 10 states, with 11 hospitalizations, according to the CDC.
Pre-cut Melon – Salmonella
In June Caito Foods recalled its pre-cut melon products after a multi-state outbreak of Salmonella Adelaide infections were traced back to the products. A total of 77 cases across nine states, with 36 hospitalizations, were reported.
Vegetable Trays – Cyclospora
In July, Del Monte recalled its vegetable trays that contained broccoli, cauliflower, carrots and dill dip following confirmed cases of cyclosporiasis in people who consumed the products. The CDC declared the outbreak over in September, with a final case count at 250 people across four states.
Salad Mix – Cyclospora
Fresh Express salad mix served at McDonalds was linked to a multistate outbreak of cyclosporiasus. The outbreak was declared over in September, with the final illness count at 511, and 24 hospitalizations.
Raw Turkey – Salmonella
Just before Thanksgiving an outbreak of Salmonella linked to raw turkey products was announced. Jennie-O Turkey Store Sales recalled more than 255,000 pounds of raw ground turkey products, however the CDC has not identified a single, common supplier that can account for this outbreak. As of the agency’s latest update on December 21, 216 cases have been reported across 38 states. The outbreak is responsible for 84 hospitalizations and one death.
Honey Smacks Cereal – Salmonella
The early summer outbreak of Salmonella Mbandaka linked to Kellogg’s Honey Smacks cereal got a lot of press, and it didn’t help that even though the company recalled the product, many retailers continued to keep the cereal on their shelves. The last illness onset was reported at the end of August. A total of 135 people were reported ill, with 34 hospitalizations.
Duncan Hines Cake Mix – Salmonella
The company recalled four varieties of its cake mixes after a retail sample tested positive for Salmonella Agbeni.
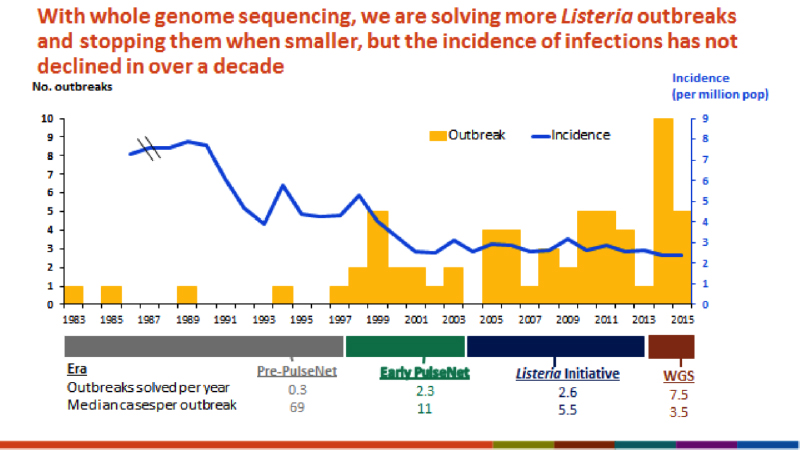
Johnston County Hams – Listeria monocytogenes
The company recalled more than 89,000 pounds of RTE deli loaf ham products over concerns of adulteration with Listeria monocytogenes.
Other outbreaks involving Salmonella this year included dried and frozen coconut, pasta salad, chicken salad and raw sprouts.