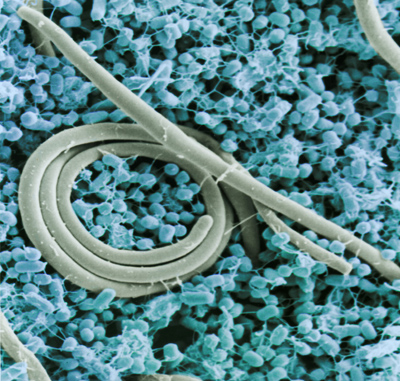
Shiga toxin-producing E. coli in dry flour, and then romaine lettuce. E. coli O104 in fenugreek sprout seeds. Recent announcements of foodborne illness outbreaks have begun involving unusual combinations of bacteria and foods. These out-of-the-ordinary outbreaks and recalls are a small but growing part of the 600 million documented food poisonings that occur worldwide every year according to the World Health Organization. Preventing outbreaks from these new combinations of pathogen and food demand a range of accurate tests that can quickly identify these bacteria. Over the past several years, outbreaks from unusual sources included:
- E. coli O121 (STEC) in flour: Last summer, at least 29 cases of a E. coli O121 infection were announced in six Canadian provinces. The source arose from uncooked flour, a rare source of such infections because typically flour is baked into final products. Eight people were hospitalized, and public health officials have now included raw, uncooked flour as well as raw batter and dough as a source of this type of infection.
- E. coli O104:H4 in fenugreek sprouts: One of Europe’s biggest recent outbreaks (affecting more than 4,000 people in Germany in 2011, and killing more than 50 worldwide) was originally thought to be caused by a hemorrhagic (EHEC) E. coli strain that from cucumbers, but was but was later found to be from an enteroaggregative E. coli (EAEC) strain in imported fenugreek seeds—the strain had acquired the genes to produce Shiga toxins.
- Mycoplasma in New Zealand dairy cows: While not unusual in cattle, the incident reported in August marks the pathogen’s first appearance in cows in New Zealand, a country known for strict standards on agricultural hygiene. The microorganism is not harmful to people, but can drastically impact livestock herds.
- Listeria monocytogenes in food sources: Listeria monocytogenes causes fewer but more serious incidence of food poisoning due to a higher death rate compared to Salmonella and Campylobacter. Whereas Listeria has been historically associated with dairy and ready to eat cooked meat products, recent outbreaks have been associated with fruit, and the FDA, CDC and USDA are conducting a joint investigation of outbreaks in frozen as well as in fresh produce.
- Listeria in cantaloupe: In 2011, one of the worst foodborne illnesses recorded in the United States killed 20 and sickened 147, from Listeria monocytogenes that was found in contaminated cantaloupes from a farm in Colorado. The outbreak bloomed when normal background levels of the bacteria grew to deadly concentrations in multiple locations, from transport trucks to a produce washer that was instead designed for potatoes.
The outbreaks underscore the fundamental need to have a robust food safety program. Bacteria can colonize many different locations and the opportunity is created by a change in processing methods and/or consumer use or misuse of products. So robust risk assessment and preventative QA procedures need to be frequently reviewed and supported by appropriate surveillance methods.
Food safety and public health agencies like the European Food Safety Authority (EFSA) or the CDC have employed a wide range of detection and identification tests, ranging from pulse field gel electrophoresis (PFGE), traditional cell culture, enzyme immunoassay, and the polymerase chain reaction (PCR). In the case of Germany’s fenugreek-based E. coli outbreak, the CDC and EFSA used all these techniques to verify the source of the contamination.
These tests have certain advantages and disadvantages. Cell culture can be very accurate, but it depends on good technique and usually takes a long time to present results. PFGE provides an accurate DNA fingerprint of a target bacteria, but cannot identify all strains of certain microorganisms. Enzyme immunoassays are precise, but can produce false-positive results in certain circumstances and require microbiological laboratory expertise. PCR is very quick and accurate, but doesn’t preserve an isolate for physicians to test further for pathogenic properties.
Identification of the pathogens behind foodborne contamination is crucial for determining treatment of victims of the outbreak, and helps public health officials decide what tools are necessary to pinpoint the outbreak’s cause and prevent a recurrence. Rapid methods such as the polymerase chain reaction (PCR), which can quickly and accurately amplify DNA from a pathogen and make specific detection easier, are powerful tools in our efforts to maintain a safe food supply.
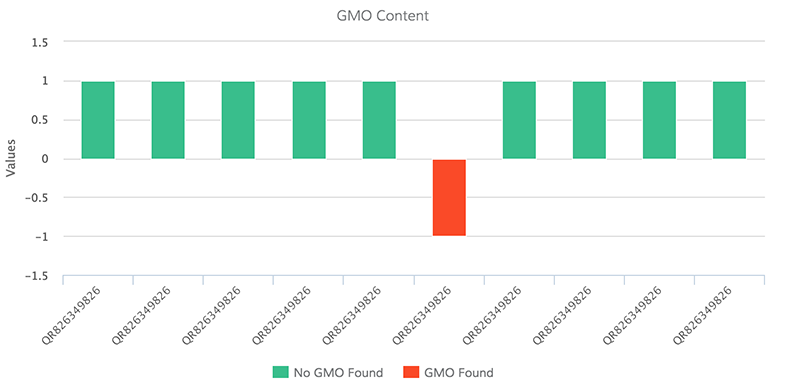
Recently, scientists and a third-party laboratory showed that real-time PCR assays for STEC and E. coli O157:H7 could detect E. coli O121, O26 and O157:H7 in 25-g samples of flour at levels satisfying AOAC method validation requirements. The results of the study demonstrated that real-time PCR could accurately detect stx, eae and the appropriate E. coli serotype (O121, O26 or O157:H7) with no statistical difference from the FDA’s Bacteriological Analytical Manual (BAM) cell culture method.
Agencies like the World Health Organization and CDC have repeatedly stated that historical records of food poisoning represent a very small percentage of true incidents occurring every year worldwide. Many of today’s most common food pathogens, like Listeria monocytogenes, E. coli O157:H7 or Campylobacter jejuni, were unknown 30 years ago. It’s not clear yet if unusual sources of contamination arise from increasing vigilance and food safety testing, or from an increasingly interdependent, globally complex food supply. No matter the reason, food producers, processors, manufacturers, distributors and retailers need to keep their guard up, using the optimum combination of tools to protect the public and fend off food pathogens.