Recent high-profile foodborne illness outbreaks appear to have an enduring impact for the entire industry – from when and how health departments respond to alleged illness to how a single tweet wreaks havoc. The bar for when a comprehensive response is required is lower and the extent and nature of the required response has changed.
Here’s what we’ve learned:
Health departments are receiving more complaints from consumers. Although much of this is believed to be related to the high-profile outbreaks, some are a result of health department websites making it easier to report illness. A few years ago, guest illness reporting required calling the health department during business hours, working your way through complex voicemail options until you reached a recorded line to leave a message about your illness. Today, most health departments in large cities and many in smaller counties, have simple on line reporting systems available 24/7. So when someone isn’t feeling well at midnight, and is sure it’s from the last thing they ate, they go online and report the illness.
Health departments are now more often following up on single reports of illness and reports of illness that are inconsistent with most foodborne illness incubation periods. This is creating a large burden for already short-staffed departments, but in response to what the public now expects. In the past, they might have replied to the ill guest and explained that they’d received no other reports, that most foodborne illness has a longer incubation period and refer the illness to personal physicians if a follow up is clinically appropriate. But today, we’re finding many health departments dispatching inspectors for even a single complaint that doesn’t appear consistent with incubation periods for that meal.
There’s increasing pressure on health departments to go public with illness events – even if the illness is no longer ongoing or creating a public health risk. The foodborne illness legal community has made it clear that they believe the public has the right to know about any and every foodborne illness. And some health departments are responding to that pressure – without their being an on-going public health risk; which would have been the trigger in the past.
Guest complaints about illness are occurring more frequently. Every single one of our clients is reporting an on-going uptick in guest reports of illness. We’re not clear if it’s that consumers are more aware of illness, more concerned or more likely to associate it with a restaurant or food service provider. But the entire industry is seeing an increase in guest reports of illness. And every guest assumes it was the last meal they ate.
How you handle any guest complaint about illness is even more critical than it was a few months ago. Here’s why: if you don’t’ respond to the guest quickly and listen with authentic empathy, that guest is far more likely than ever before to tweet about you, write a bad review, post on social media or contact the media. You need to act quickly and it doesn’t matter if it’s a weekend or holiday. Waiting until Monday morning is not an option.
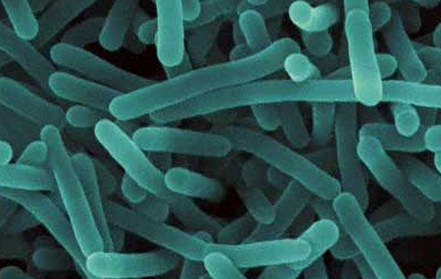
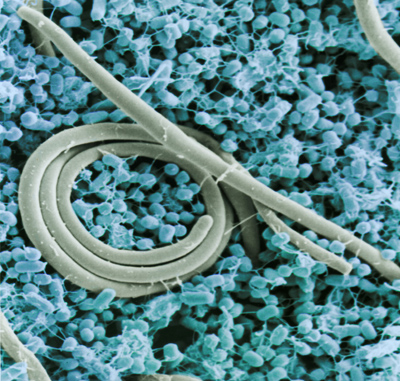
Noro season is year-round now… it’s no longer the winter vomiting disease like it is called in some places. Noro virus outbreaks continued in California (and elsewhere) until after the school year ended. We need to be alert to Noro all of the time.
Fourth of July
Fourth of July was an unusually quiet day in the restaurant, quieter than anticipated (meaning more prep done than needed). The next day, two employees called out sick. A day later, two guests (small parties) called the restaurant reporting illness and later that day, two more larger parties emailed their reports of illness through the corporate website. It took another 24 hours to match these multiple illness reports through three different channels. It didn’t trigger a full-blown response and implementation of the noro sanitizing protocol.
THE FINAL TALLY: 40+ guests reporting sickness and nearly half of the staff.
THE LESSON: Coordination of reporting mechanisms so that you see a potential problem and respond at the earliest point when you can have the greatest impact in minimizing risk.
Employees continue to work sick. There are so many reasons that employees work sick and it has little or nothing to do with paid sick time. They work sick because they’re not very sick, they don’t understand that any gastrointestinal upset may be a sign of foodborne illness, they don’t want to disappoint their manager or they don’t want to let their team down. They’re working sick for altruistic reasons without understanding the potential ramifications. We have a long way to go in educating managers and employees about what “sick” looks like, what can happen from working sick and why we need to work together long term to change this set of behaviors.
Employee Exclusion Policies need to be revisited. Someone is shedding the Noro virus for twenty-four hours prior to become symptomatic and then at very high levels for three days after symptoms end. Sick employees need to be excluded for much longer than they currently are in most restaurants and food service establishments to control Noro outbreaks.
Employee Illness on Days Off are as critical to crisis prevention and response as illness on work days. You need to know if an employee was sick on a scheduled work day or on a day off. As we discussed previously, they were shedding the Noro virus before they got sick and for days after. Your illness response plan needs to include a very robust tool for employee illness reporting – one that is as easy to use seven days a week and raises an alert to management when there are two or more sick employees.
It’s time to redraft and recommunicate the definition of a potential crisis in your organization. In the past, we previously used the following definitions of what defined a potential crisis for a restaurant or foodservice group:
- Two or more employee illness reports (for same time period and symptoms)
- Two or more guest complaints (from different parties for same time period)
- One confirmed employee illness (with a communicable disease)
Your new definition must be broader and reflect the lower trigger points for action. It may include one guest complaint from a large party, illness in a neighboring school, social media buzz about illness from your location and / or a health inspection in response to a guest complaint of alleged illness.
The takeaway: the lessons learned continue to evolve and new ones emerge with each new outbreak. Making sure we identify and share these lessons across the industry and your organization is critical for being prepared to first identify and then quickly respond to the next threat that comes your way.